Why I reach for iQ instead of my stethoscope.
Introducción
There are few things as unnerving as watching a patient struggle to breathe. While a systematic approach to the assessment and stabilization of airway, breathing and circulation helps to frame our management of these patients, there is still an inevitable sense of urgency and danger when a patient presents with severe dyspnea. While some interventions are ubiquitous (cardiac monitoring, oxygen, IV access), many of the disease processes that result in severe shortness of breath call for dramatically different treatments in order to correct the underlying issue(s):
A patient with:
- Heart failure and pulmonary edema may need a combination of afterload reduction, positive-pressure ventilation, diuresis, and inotropic support.
- Severe emphysema may require inhaled beta-agonists, corticosteroids, positive-pressure ventilation, fluids and antibiotics.
- A massive or pulmonary embolism needs anticoagulation and consideration of systemic or targeted thrombolysis, thrombectomy or ECMO.
- A pneumothorax and severe dyspnea needs a tube thoracostomy, and a patient with a large pleural effusion needs a thoracentesis or tube thoracostomy.
- Cardiac tamponade needs IV fluid support and a pericardiocentesis or pericardial window.
- Pneumonia needs antibiotic therapy, supplemental oxygen, fluid resuscitation and sepsis assessment/management.
While auscultation with a stethoscope may narrow the field of possible diagnoses, there is still a great deal of overlap in how these diseases sound to the ear. Acute pulmonary embolism, acute decompensated heart failure and acute emphysema may all result in diffuse wheezing. Then again, cardiac tamponade and pulmonary embolism may both present with clear lung sounds. Diffuse abnormal lung sounds may be a result of multilobar pneumonia, pulmonary edema, or pulmonary fibrosis.
The human brain devotes 20-40% of function to vision and visual-spatial processing and only 3% to auditory function. Is it a surprise that we learn more about our world (or our patients) by looking instead of listening? Ultrasound allows us to transduce high frequency sounds into a visual picture, and in that capacity provide us with a stream of information that we are naturally inclined to process more keenly.
There is a wealth of evidence demonstrating the superior diagnostic performance of ultrasound imaging of the heart and lungs over auscultation of either of these vital organs (see references below). Now that I can carry an imaging tool in my pocket, I can’t find a reason to use a less accurate device, especially when I’m standing there looking at someone gasping for air.
Exploración con imágenes
A rapid POCUS assessment of the heart and lungs can be performed in less than a minute, and typically includes parasternal, apical and subcostal cardiac views, as well as anterior and lateral lung views.
Complete descriptions of technique and common findings can be found here, but some representative images from Emergency Department patients with severe shortness of breath are shown in Figures 1-4.
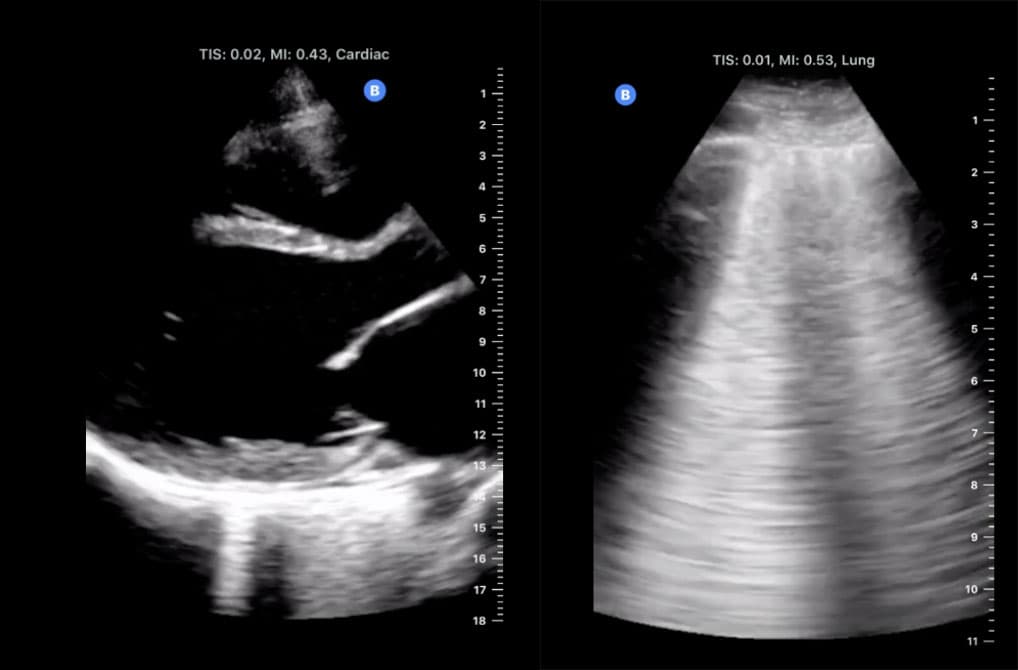
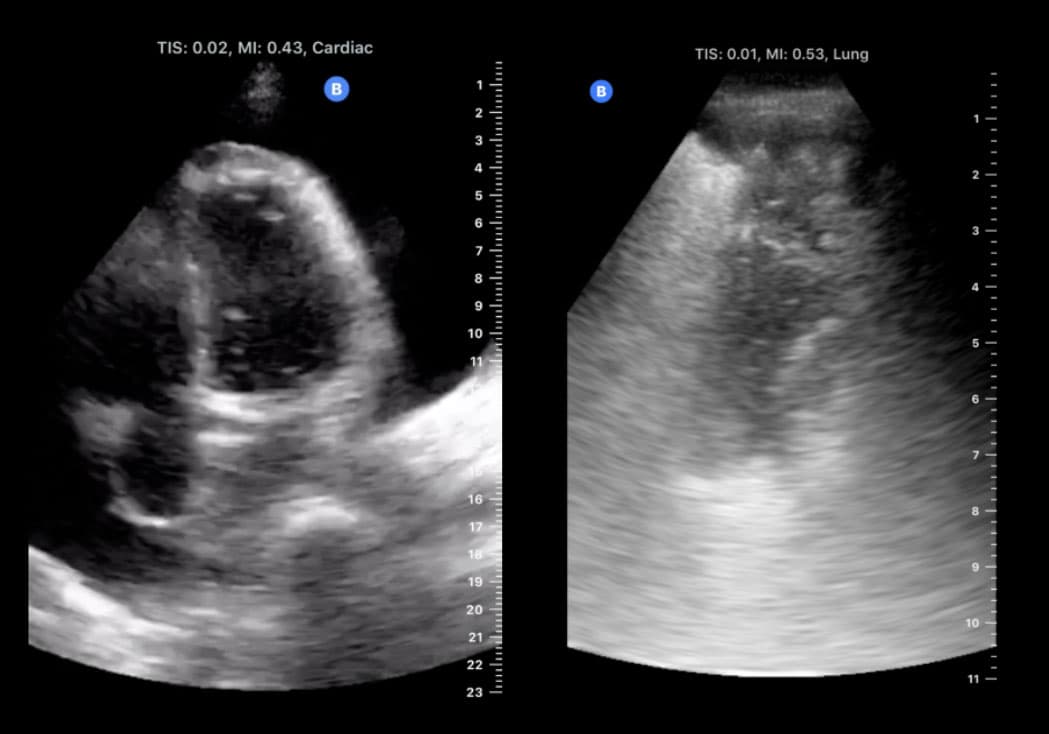
Fig 4. Demonstrates a dense subpleural consolidation in a septic patient with lobar pneumonia.
What Does This Teach Us?
Point of care ultrasound is easy, safe, effective, and diagnostically superior to auscultation in the assessment of patients with severe shortness of breath. It’s time to start capitalizing on our innate predisposition to visual processing, and to look rather than listen to these patients who need our immediate treatment.
References
Kobal SL1, Trento L, Baharami S, et al. Comparison of effectiveness of hand-carried ultrasound to bedside cardiovascular physical examination. Am J Cardiol. 2005 Oct 1;96(7):1002-6.
Pivetta E, Goffi A, Lupia E, et al. Lung Ultrasound-Implemented Diagnosis of Acute Decompensated Heart Failure in the ED: A SIMEU Multicenter Study. Chest. 2015 Jul;148(1):202-210.
Zanobetti M, Scorpiniti M, Gigli C, et al. Point-of-Care Ultrasonography for Evaluation of Acute Dyspnea in the ED. Chest. 2017 Jun;151(6):1295-1301
Image 1. Normal Side. Pediatric Lung setting, demonstrates clear pleural line with sliding and z lines (aka comet tails). No indication of B lines; normal appearing lung
Image 2. Abnormal side. Additional air bronchograms further identifying the consolidated lung region. With respiration consolidated lung is partially obscured by B lines. Consolidated lung with dynamic air bronchograms
Image 3. Abnormal Side. On left of image: few B lines indicating presence of fluid in lung, irregularly appearing pleural line with sub pleural consolidation (~ 2 cm in depth). Consolidated lung area looks like liver hence the term, lung hepatization. Echogenic dots are air bronchograms; these collections move with respiration therefore they are called dynamic air bronchograms. (Note: dynamic air bronchograms = pneumonia; static air bronchogram - no movement with respiration = atelectasis)